Endodontic Services
All about microscopic endodontic treatment
Endodontics is a specialty of dentistry that deals with “treating the canals” (infections, inflammation, toothache pain or emergencies).
Endodontic treatment under a microscope can save a tooth for life.
Endodontic treatment is performed by an endodontic doctor, an endodontic specialist.

Dental microscope
The microscope can be used successfully in almost all dental procedures, as it offers the possibility to visualize details that cannot be observed with the naked eye, but which can be of considerable importance for diagnosis and for the performance of a quality dental treatment.
In our clinic, Ortho Implant Center Cluj-Napoca, a ZEISS microscope is used.
As the name suggests – formed by the juxtaposition of two Greek terms, namely: “endo” which translates to “inside” and “dont” by “tooth” – endodontic (or canal) treatment can be defined in a very general way as the treatment of the inner part of the tooth.

Zeiss Microscope – Ortho Implant Center Clinic Cluj-Napoca:

Ortho Implant Center Cluj-Napoca – ZEISS microscope
What does the dental microscope help us with?
In endodontics, however, the use of the microscope is no longer a matter of choice. As already mentioned, root canal treatment, or endodontic treatment, involves removing the pulp from the pulp chamber and root canals, as well as thoroughly cleaning them. It should be noted that the teeth can have from one to three roots, with up to three root canals each, and some of these canals can be as thin as a hair. For root canal treatment to be effective, it is important to detect and treat all root canals. For these reasons, in this type of treatment the microscope is an indispensable tool, as it allows:
- identification of all channels
- identification of channel inlet holes
- identification and treatment of calcified canals
- identification of root perforations and their sealing
- detection of root fractures
- view and remove broken needles from channels
- restoring incorrect canal treatments
- Adequate and thorough cleaning of the channels for sealing and sealing.
Healthy tooth – decayed tooth
To help you visualize and understand exactly what happens to a healthy tooth that becomes ill, requiring canal (or endodontic) treatment, we include below an image that summarizes the anatomy of a healthy tooth (fig1), by contrast with the anatomy of the affected tooth (fig.2):
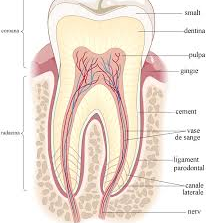
Fig. 1 Healthy tooth
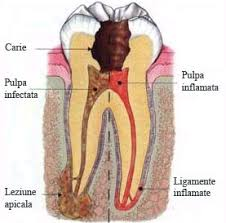
Fig.2 Tooth affected by caries
As can be seen in the image above, viewed from the outside to the inside, the tooth consists of several “layers”. Thus, just below the outer enamel there is a hard layer called dentin, and inside it a soft tissue called pulp. It contains blood vessels, nerves and connective tissue, and has a formative, nutritional and sensory role, ensuring, among other things, the sensitivity of the tooth. Occupying a fairly large area, the pulp extends from the crown (where it is contained in the space known as the pulp chamber), to the top of the roots (in the root canals). It is normally protected from harmful factors by the three layers that surround it, namely: enamel, dentin and cement, but if these protective layers are perforated for various reasons (deep carious lesions, repeated treatments of the tooth in cause, cracks, etc.), the microbes in the saliva will infect the pulp, first the coronary one and then the root one, causing pain or dental abscess.
At this point, the required treatment is the endodontic one, through which the inflamed or infected pulp is carefully removed, and the inside of the root canal is cleaned and shaped, which is then perfectly sealed.
Questions and answers
During the growth and development of the tooth, the pulp has an essential role, because, at this stage, it fulfills, in addition to the formative and sensory role, also a nutritional role. However, once the tooth reaches maturity, it can survive without dental pulp, as it will continue to be fed by the surrounding tissues. Therefore, removing the pulp of a mature tooth does not present any major risks in the short or long term.
If the inflamed or infected pulp of the tooth is not removed in time, the pathology will worsen, the pulp will die, causing the formation of pulpal gangrene, and the hard tissues and supporting tissues will also gradually deteriorate, which will eventually lead to tooth loss. In addition, there is a risk that the infection will spread to the bone, causing significant damage and increasing the risk of complications.
Such signs may include, but are not necessarily, pain: prolonged sensitivity to heat or cold, sensitivity to touch and chewing, tooth discoloration, swelling, tenderness in the lymph nodes, and near bone and gingival tissue. However, there are also situations in which the patient does not show any symptoms.
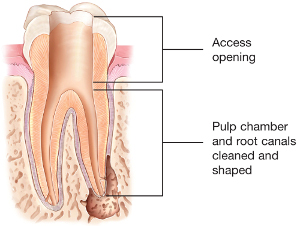
Stages of endodontic treatment
Any effective treatment involves both establishing a correct diagnosis and monitoring the effectiveness of therapy. Since, as we have shown above, endodontic treatment is a treatment of the inside of the tooth, ie of a part that cannot be observed directly, in this case, the only way to establish the diagnosis and monitor the therapy is based on the realization of the at least three dental radiographs, namely:
1. The initial radiograph, on the basis of which the diagnosis and the therapeutic conduct will be established.

Initial orthopamtomogram radiograph (OPT OR OPG), which can be performed at our Ortho Implant Center clinic. See Radiology Rates.
2. The second x-ray, which you will perform during treatment, to monitor the effectiveness of the intervention.

3. Final control radiograph, which is performed at
end of treatment.

Sometimes conventional (2D) radiography is not enough for a proper diagnosis. The endodontist needs to see better inside by requesting a 3D x-ray or a CBCT.
Dental CBCT can be performed at our clinic, Orho Implant Center. See Radiology Rates.
There is a concern among patients about the risks involved in performing repeated dental x-rays. It must be said that the high-performance radiological equipment currently used exposes the patient to a minimum dose of radiation, which does not justify such fears.
Duration of endodontic treatment
Although endodontic treatment can be performed in a single visit, for optimal results, in some cases it is preferred to perform it in two separate sessions, a few days apart. Depending on the pathology, other additional canal treatment sessions may be necessary, especially when we have major difficulties such as fractured instruments, perforations or large apical infections.
1. Once the x-ray is examined, the endodontist administers a local anesthetic, isolates the tooth by placing a protective “foil” called a “dam” to keep the tooth clean during the procedure, preventing its contamination by microbes and bacteria in saliva. Through an open hole in the crown of the tooth, the pulp is carefully removed from the pulp chamber and from all the root canals, which will then be cleaned and shaped.
2. Once the pulp has been removed, an empty space remains in the root canals and in the pulp chamber, which must be sealed and sealed; otherwise, this space would be immediately populated by bacteria. Sealing is performed by a process known as hot vertical condensation, using a non-absorbable and compact biocompatible material, known as gutta-percha, together with an adhesive cement, or sealer. This process ensures a homogeneous filling as well as lasting results.
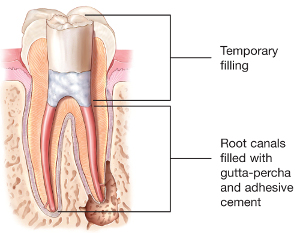
3. After the endodontic treatment, the coronary restoration of the tooth will be necessary, so that it can resume its functionality. The dentist will complete the treatment by making a permanent filling.
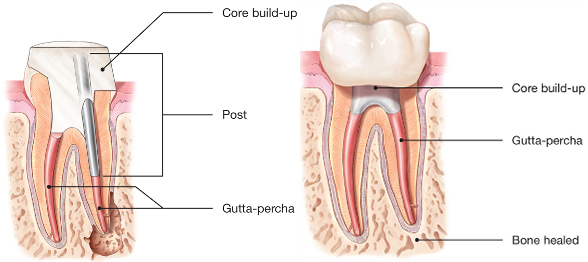
Most of the time, however, a tooth that requires endodontic treatment has a compromised crown. In these situations, simple filling is not enough. The dentist will place a fiberglass pivot inside the tooth, thus increasing its strength, after which the resistance structure and aesthetics of the tooth are restored by metal-ceramic crowns, zircon-ceramic or all-ceramic, inlays (inlay, onlay or sheet top) .it is absolutely necessary the next step (prosthetic restoration) after a canal treatment. See Prosthetics.
When the endodontic treatment is performed in two sessions, the orifice at the level of the dental crown can be sealed with a temporary material in a first phase, which will then be replaced with a permanent filling at the end of the treatment.
Recommendations after endodontic treatment
Pain, tooth sensitivity
After a canal treatment, some lower or higher sensitivities (pains) may appear. Your endodontic doctor will prescribe the appropriate medication for your case.
It is normal for pain to occur – from simple embarrassment, sensitivity to pain that only subsides to analgesic or anti-inflammatory medication.
Antibiotics may be prescribed / recommended in some cases, but it depends a lot on the initial diagnosis and the clinical situation present. The endododnt doctor is the one who can prescribe antibiotics.
We are waiting for you in our clinic
Ortho Implant Center from Cluj-Napoca!

